Chronic kidney disease (CKD) is a nasty condition, and a common one. It affects about 10% of adults globally – that’s more than half a billion people – and according to the World Health Organization, it’s responsible for 1.5% of all deaths worldwide. In Hong Kong, about 800,000 people have CKD, with people in low-income communities particularly likely to be affected; in 2022, kidney diseases were the seventh most common cause of death in the city. CKD can lead to kidney failure, meaning dialysis or transplantation is needed, and it’s also associated with a high risk of cardiovascular diseases.
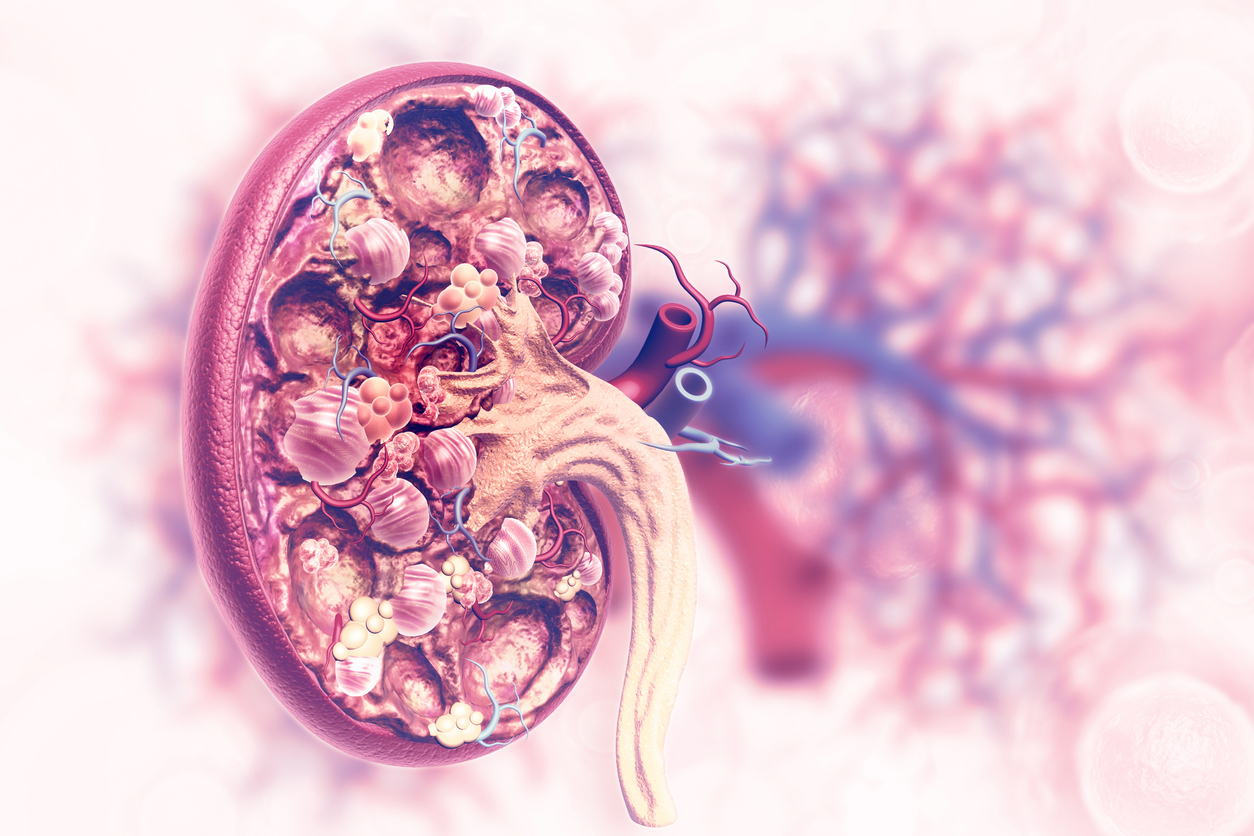
One marker of CKD is prolonged kidney fibrosis, in which the kidneys are scarred and cannot remove metabolic waste and toxins from the blood properly.
“Fibrosis occurs when wound healing is deregulated, leading to the formation of scar tissue in the kidney,” says Professor Jonathan Choi Chung-hang, Associate Professor in the Department of Biomedical Engineering at The Chinese University of Hong Kong (CUHK)’s Faculty of Engineering. “Kidney fibrosis is a common pathological feature of CKD. All CKD patients have some degree of kidney fibrosis, and patients with kidney fibrosis are considered as CKD patients.”
The problem is, there are currently no specific treatments for kidney fibrosis. There are some medicines that can slow the progression of the disease, but their effectiveness is limited, and they can cause side-effects such as hypotension, aka low blood pressure, and hyperkalemia, meaning abnormally high potassium levels.

That might be about to change. A CUHK research team led by Professor Choi, which also included first author of the research paper Dr Cecilia Chan Ka-wing, plus Professor Szeto Cheuk-chun and Professor James Lau Yun-wong, has conducted successful experiments on mice using folic acid-conjugated gold nanoparticles – conjugation in chemistry refers to a chemical linkage between two different substances – that may offer a safe, effective treatment for the condition.
Nanomedicines show promise for treating a disease, but there’s a challenge in getting them to the right spot in the kidney where the problem is. Previous attempts used large nanoparticles; despite their small size, they were too big to pass through the kidney’s natural filter. The recent study used smaller gold nanoparticles (around 7 nm), coated with folic acid molecules. These folic acid molecules help the nanoparticles target the specific areas in the kidney where they’re needed. The nanoparticles treat the disease by blocking an enzyme called p38α MAPK, which is involved in its development. Importantly, these nanoparticles can be easily removed from the body without causing harm.

The team first started looking for a nanomedicine to treat renal fibrosis in 2016. In addition to gold nanoparticle and folic acid, their original formulation also included therapeutic gene cargoes, which they thought would be effective against the disease. But unexpectedly they discovered that the gold nanoparticle was sufficient to inhibit the p38α without chemical or biological drugs.

There are some other chemical inhibitors of p38α MAPK that have been tested in humans, but they haven’t been approved due to concerns over their potential toxicity. Previous candidates for a potential treatment required multiple injections, but the team discovered that a single injection of these gold nanoparticles could effectively treat the condition. The timing is important: previous treatment candidates were also solely preventive, but CKD is asymptomatic in its early stages, meaning patients are mostly diagnosed when they’re already suffering from the condition, so reactive rather than preventive treatments are more effective.
The ultimate hope is to offer a safe, effective gold nanomedicine. So far, the team has tested theirs in mice. The next stage, says Professor Choi, is to continue the clinical trial process.

“In this work, we have shown the safety and efficacy of our nanoparticle in mice. We will have to evaluate the long-term safety of the nanoparticle in large animals, say dogs or monkeys. After that, we can apply for clinical trials to test its safety and efficacy in humans.”