The Chinese University of Hong Kong (CUHK)’s researchers continue to search for ways to fight some of the world’s most widespread diseases more effectively. Indeed, research that advances the fight against major diseases is one of most important real-world applications of the university’s academic excellence. Now, three new developments promise a brighter future for sufferers of three of the commonest and most debilitating conditions of all: diabetes, stroke and hepatitis B.
Decoding diabetes
Diabetic kidney disease (DKD) is one of the many negative outcomes associated with diabetes, which causes almost half of renal failure cases in Hong Kong. It happens when high blood sugar levels cause damage to the blood vessels within the kidney, and it’s extremely serious: it can cause kidney failure, and it also seems to be associated with cardiovascular disease risk, although it’s unclear exactly how. Indeed, cardiovascular disease often causes death among kidney patients.
DKD prognosis remains poor due to factors including younger onset of age, the high prevalence of elevated blood pressure among those with diabetes, low awareness of the dangers of DKD and its lack of symptoms, low rates of early detection and increasing obesity.

Help is at hand, though, thanks to a new study led by CUHK’s Faculty of Medicine (CU Medicine). Looking at 1,991 people from the Hong Kong Diabetes Biobank, it identified 156 metabolites associated with DKD, as well as isolating 22 of them that also have a meaningful association with cardiovascular disease. Include triglyceride-rich lipoproteins, small high-density lipoprotein, leucine and albumin, they can be identified using blood tests.
The study will allow medical professionals to better predict cardiovascular disease and tailor treatments accordingly. “Identifying those at increased risk should alert clinicians to manage these cases more intensively and ensure better control of risk factors, as well as appropriate use of kidney protective treatments to slow the progression of DKD,” says Professor Ronald Ma, S.H. Ho Professor of Diabetes and Head (Academic Affairs) in the Division of Endocrinology and Diabetes at CU Medicine.
The nanorobot wars
Stroke is the world’s second most common cause of mortality, accounting for 11% of all deaths. A treatment called a tissue plasminogen activator, or tPA, can dissolve the blood clots that cause the condition, a process known as thrombolysis, but the problem is targeting: current methods of distribution of high-dose tPA mean that the drug is spread all over the body, diluting its effectiveness and minimising the dose that can be administered (as it poses a risk of systemic and brain hemorrhage during treatment). That means it works more slowly – and in the meantime, 1.9 million brain cells are dying per minute from stroke onset. So it would be really handy to be able to target the affected area more precisely.

That could soon be possible, thanks to a new technology developed by a group from the Department of Imaging and Interventional Radiology and the Department of Medicine and Therapeutics at CU Medicine, with the Department of Mechanical and Automation Engineering in the Faculty of Engineering. “It consists of minuscule magnetic robots (called tPA-nbots) loaded with tPA that can be guided to the exact site of the stroke and administer a precisely targeted dose of the drug. Just 200 to 300 nanometres in size – that’s 0.0002 to 0.0003 millimetres – they can dissolve clots five to 20 times faster than the traditional treatment,” says Professor Zhang Li, Professor in the Department of Mechanical and Automation Engineering.
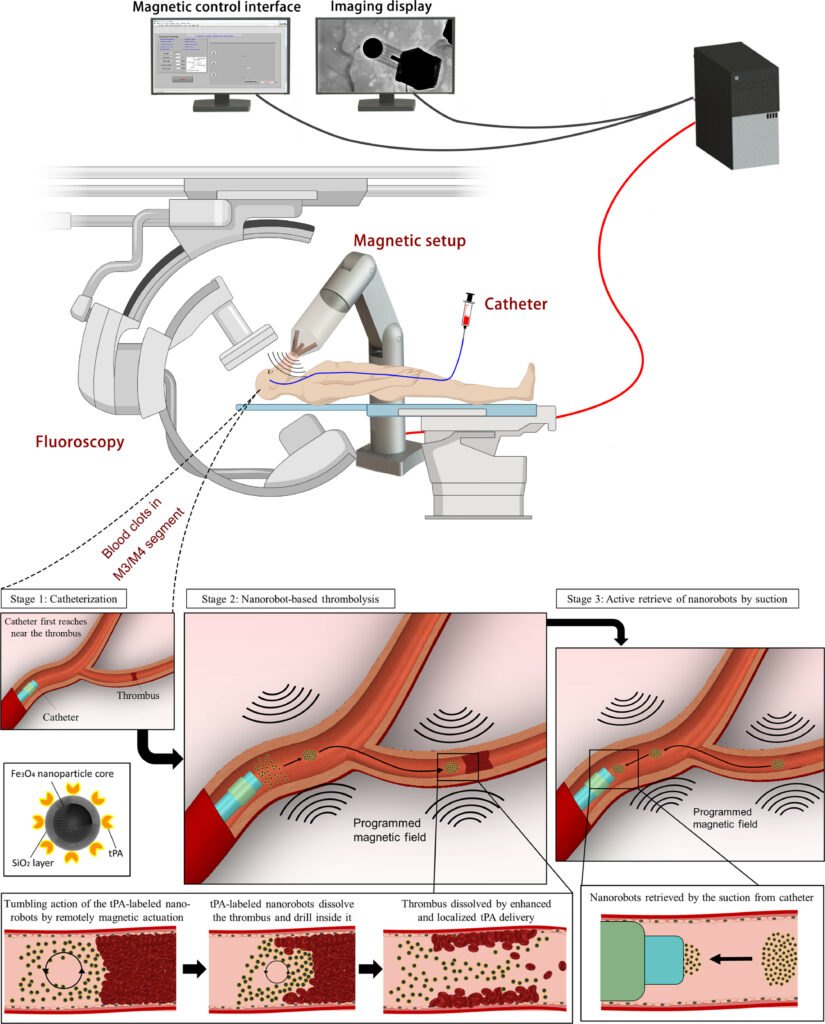
To further refine the technique, says Professor Thomas Leung Wai-hong, Head of the Division of Neurology and Lee Quo Wei Professor of Neurology in CU Medicine’s Department of Medicine and Therapeutics, “We need to develop a real-time, large-field tracking system that visualises the interaction between nanorobots, blood clots and the blood environment; efficiently retrieve nanorobots from brain blood vessels after clot dissolution; and minimise the disintegration of nanorobots when exposed to high arterial blood flow.”
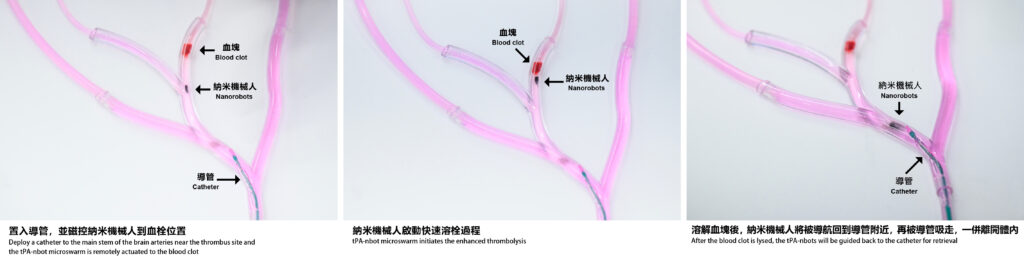
In a further useful development, the team also used a technique known as using laser speckle contrast imaging (LSCI) to monitor the robots and their impact on clots in animal models, allowing researchers to refine the treatment. “It elucidates nanorobot behaviour under different nanorobot dosages, magnetic strengths and angles in animal studies, which are crucial parameters to be optimised before human implementation,” says Dr Bonaventure Ip Yiu-ming, Assistant Professor in the Department of Medicine and Therapeutics at CU Medicine.
Giving hepatitis sufferers a break
Hepatitis B can lead to a range of potentially fatal outcomes, including cirrhosis, liver failure and liver cancer. Moreover, the virus that causes it is present in about 6.2% of the Hong Kong population, or about 465,000 people. Antiviral treatments such as entecavir (ETV) and tenofovir disoproxil fumarate (TDF) are effective at suppressing the virus and reducing the risk of negative outcomes – but like all medications, they can have side-effects, particularly given that they’re typically used for extended periods, even lifelong.
A new CU Medicine study of more than 40,000 patients with chronic hepatitis B aged 60 or above over an eight-year period found an increased risk of fractures in people taking TDF, caused by loss of bone density. The difference between two drugs becomes apparent after two years, and sits at a cumulative 50% after eight years.
TDF use is also associated with decline in kidney function, but it may be more effective than ETV in reducing the risk of liver cancer from hepatitis B. However, tenofovir alafenamide (TAF), a new generation of tenofovir, could be an alternative.

“TAF is a newer generation of tenofovir that is more stable in the body, so it can be designed and taken at a lower dose while still being effective,” says Dr Terry Yip Cheuk-fung, Associate Professor in the Department of Medicine and Therapeutics, CU Medicine and Deputy Director of Medical Data Analytics Centre. “Using TAF instead of TDF can reduce kidney and bone toxicity.”
The study underlines the need for doctors to take a holistic view, reviewing patients’ overall health condition and taking it into account when prescribing hepatitis treatments.










