Infection rates from COVID-19 around the world are rampant, with over 160 million confirmed cases recorded. This makes it essential to develop drugs which are fast and effective in treating patients. An international research team led by the Faculty of Medicine of The Chinese University of Hong Kong (CU Medicine) and LKS Faculty of Medicine of The University of Hong Kong (HKUMed) has recently discovered a new role for the retired hepatitis C drug “Simeprevir”, which is to effectively suppress the SARS-CoV-2, and the outlook is optimistic.
Currently, COVID-19 patients are treated for the most part by the “cocktail therapy”, a triple combination of drugs, but those who are seriously ill or with respiratory failure are prescribed injections of remdesivir. While remdesivir is effective, it only targets one major viral protein RNA polymerase, meaning that remdesivir-resistant viral mutants may emerge, and it does not reduce the death rate.

To meet this urgent medical need, Professor Billy Wai Lung Ng, Assistant Professor of the School of Pharmacy, CU Medicine and Dr. Michael Chi Wai Chan, Associate Professor of the School of Public Health, HKUMed collaborated with over 30 scientists from local and overseas laboratories to search for a more effective drug molecule for the treatment of COVID-19, in early 2020.
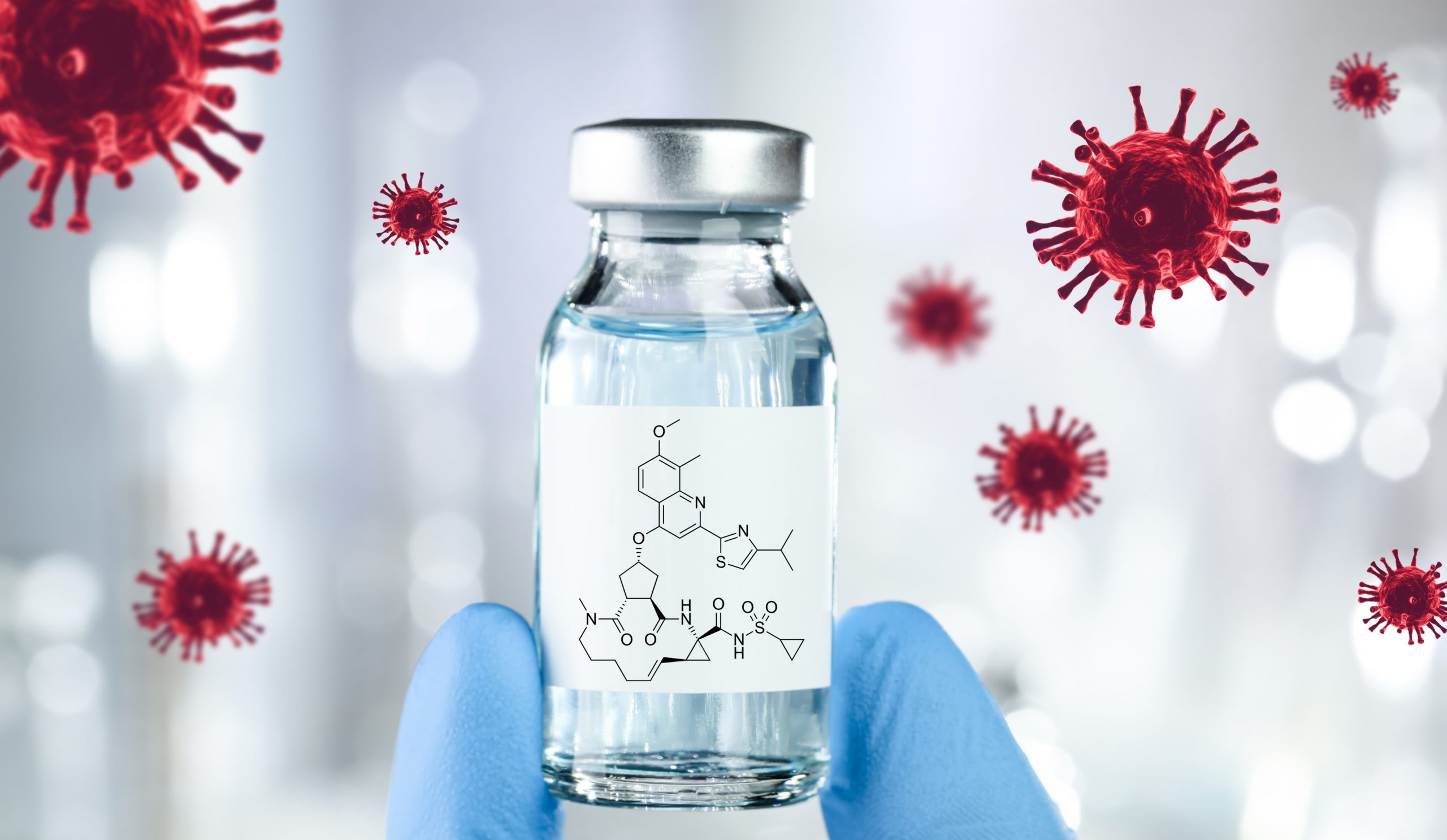
The team tested a number of antiviral drugs approved by U.S. Food and Drug Administration (FDA) in a cellular infection model, and eventually discovered that “simeprevir”, an oral hepatitis C virus drug, can simultaneously target two major viral proteins (main protease Mpro and RNA polymerase), give a potent response to the virus and strongly suppress the replication of SARS-CoV-2. It is by now the only antiviral drug that can target more than one SARS-CoV-2 protein and remain effective even if one of the proteins becomes mutated. A combination of simeprevir with remdesivir can result in drug synergism and generate an even more effective outcome with fewer side effects. Crucially, this synergy is also effective against feared virus strains such as N501Y and E484K.
The viral infection experiments at the P3 laboratory in HKUMed demonstrated that combined equal doses (3.3uM) of remdesivir and simeprevir increased the antiviral effect by over 100-fold when compared with remdesivir alone. Approximately 90% of virus reproduction was inhibited. This not only means that the therapeutic possibilities for simeprevir are greater, but it also gives a clearer view of the interplay between the drugs, which can open up additional ways into fighting the virus.

Professor Billy Ng elaborated, “Though simeprevir has already been replaced by other treatment methods for hepatitis C patients, the repurpose of existing FDA-approved therapeutic agents can shorten the time frame for clinical trials and may reveal new drug targets that can be further exploited. The cost of producing the drug is expected to be lower as the most expensive R&D part has been passed. This is indeed a very promising and encouraging discovery,” he added, “The drug is now undergoing animal testing, and discussions are beginning with pharmaceutical companies about its prospects for mass production. It is expected that the preliminary results are likely to come through in between six months and a year. Clinical testing will follow and then, if successful, it can be used.”

Professor David Shu Cheong Hui, Stanley Ho Professor of Respiratory Medicine at CU Medicine said, “When COVID-19 patients develop respiratory failure, remdesivir is the only effective drug. However, remdesivir is an expensive drug which is difficult to buy and does not help to reduce the death rate. The discovery of simeprevir may be a hope for reducing the death rate.” Professor Hui also looks at the importance of developing treatment like this for beyond the present pandemic, “With the development of new vaccines, there seems to be light at the end of the tunnel for the COVID-19 pandemic. However, the virus remains rampant and the recurring coronavirus epidemics in the last two decades suggest that the virus may become a persistent healthcare issue threatening global health. It is therefore essential to enlarge our therapeutic box in preparation for future coronavirus pandemics.”
CU Medicine research teams have lately been in the forefront of discovering and proposing solutions to unanticipated consequences of the COVID-19 outbreak. Last year, another international research team led by Professor Billy Ng has reviewed the molecular basis of coronavirus RNA proofreading mechanism, and evaluated the nucleoside analogues and nucleic acid-based therapies that could be used either individually or in combination, to target the relevant mechanism, while a study in May this year analyses the key nucleic-acid based technologies against coronavirus, and explore the combination therapies of them with other antiviral drugs for a better outcome.