You might think of myopia as a relatively trivial condition; after all, lots of short-sighted people just wear glasses and get on with their lives. But its implications can be profound. Myopia is caused by elongation of the eyeball, a process that is irreversible once it has started; even laser refractive surgery has no impact on the root cause of the condition.
“The eyeball is just like a camera,” says Dr Jason Yam Cheuk-sing, Associate Professor from CUHK’s Department of Ophthalmology and Visual Sciences, Faculty of Medicine (CU Medicine) and Director of the CUHK Jockey Club Myopia Prevention Programme. “As the eyeball gets longer and longer, the retina, which is like the film, will become stretched.”
Particularly in adulthood, myopia can lead to a range of conditions that seriously impact sight, including glaucoma, macular degeneration, retinal detachment and cataracts. Medical emphasis has to be on preventing it.
Myopia rates, moreover, are increasing globally, currently affecting about a third of the world’s population, a figure that could be set to increase to about half by 2050, according to an estimate from the American Academy of Ophthalmology. Rates are higher in East Asia than other regions, and they’re particularly high in Hong Kong.
“The myopia rate in Hong Kong is one of the highest in the world,” says Dr Yam. “Myopia is an interaction between the environment and genetic factors. For parents who have high levels of myopia, the risk in their children is 12 times higher – and in China, the genetic factors are probably stronger. Among environmental factors, one is where outdoor time is not enough, and the second is more near work.”
Both of those factors, of course, were exacerbated by the Covid-19 pandemic. There was an exaggerated change of lifestyle. In Hong Kong, school children’s outdoor time decreased from an average of 1.4 hours to 0.4 hours during the critical Covid period, and their screen time went from 2.5 hours to 7 hours. Therefore the development of myopia has jumped. Recent data shows that before Covid, 13% of children were myopic at six years old; after Covid, it’s 25%.
Spending more time outdoors has been shown by previous trials to be an effective treatment, but enforcing that kind of thing can be tough, particularly in the context of Hong Kong, where children often lack opportunities to experience the outdoors, and the pressure to stay indoors and study can be intense. As every parent knows, trying to get children to put their electronic devices down is generally a losing battle – and in future that’s only likely to head in one direction.
The LAMP2 study, for which Dr Yam was the Principal Investigator, offers another possible solution. The groundbreaking research, conducted between 2017 to 2020 at CUHK Eye Centre, gave 474 children aged four to nine years, who were not myopic themselves but have at least one myopic parent, a nightly dose of atropine eyedrops: some at a concentration of 0.05% and others at 0.01%, while a third group were given a placebo.
Atropine has been used as a treatment foy myopia for decades, but not as a possible way to prevent its onset, and previously only in much higher concentrations of about 1%. The problem with that is the common and fairly unpleasant side-effects it can cause: severely dilated pupils that make it hard to see anything close up, and photophobia, or discomfort in bright light. As a result, 1% atropine is not commonly used as a daily treatment.
LAMP 2 showed that the 0.05% atropine drops resulted in the incidence of myopia falling by 46.4% over two years; the 0.01% solution produced no significant effect, demonstrating that the treatment is concentration-dependent.
“It’s the first study to demonstrate a high efficacy in preventing myopia,” says Dr Yam. “It shows atropine doesn’t just prevent progression but is also an effective way to prevent onset.”
The treatment is mostly likely to benefit high-risk children – those whose parents suffer from serious myopia, particularly in cases where both of them do. Babies are born long-sighted, and assessing the level of the so-called hyperopia reserve that remains with them in childhood provides another useful tool for working out which children should receive the eyedrops.
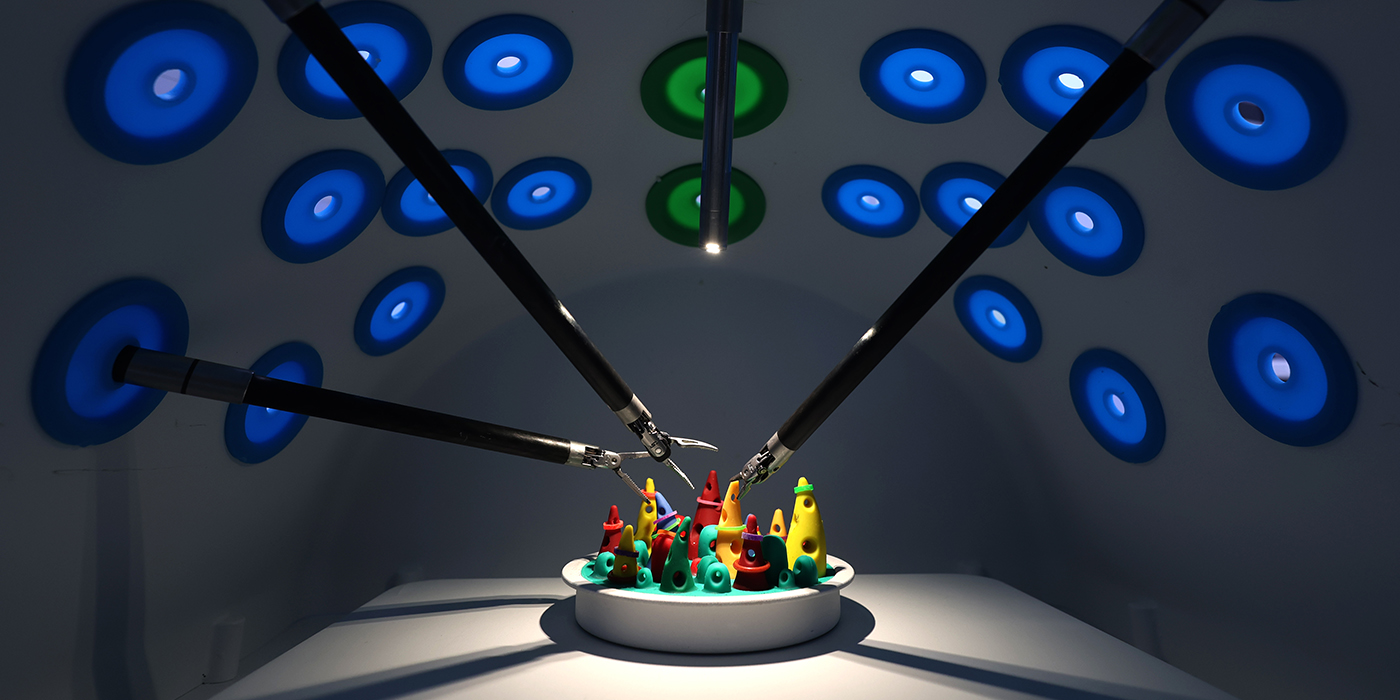
The next stage for the treatment is to combine it with red light therapy, another treatment that has shown promising signs in studies in mainland China of being able to control the onset of myopia. The LAMP3 study will compare the effects of the two therapies both separately and in combination on the development of myopia in 500 children in Hong Kong. After that, LAMP4 will look at their impact on the condition’s onset.
“What we’re really keen to do is increase the efficacy to 80 to 90% or even higher,” says Dr Yam. “We can effectively reduce high myopia in generations. It’s very important to prevent future blindness.”