When cancer metastasises, forming new tumours in other parts of the body, the lungs are one of the most common places to be affected. Unfortunately, those metastases are really hard to treat.
Highly invasive surgical resection
Currently, an important treatment option is surgical resection of the affected areas. Surgery can be a highly invasive procedure, with all the potential complications, that can include wound infection, surgical bleeding and air leaks. Surgical resection also results in healthy lung tissue being removed, which can cause a long-term reduction in lung capacity in people who could really do without that additional burden on their health. In addition, the operation is most often performed on people with advanced stage cancer, who are often already weakened by the side-effects of treatments such as chemotherapy. Furthermore, patients frequently have multiple metastases spread throughout their lungs, so that these potential dangers of surgery can be multiplied several folds.
A non-invasive and effective transbronchial microwave ablation of lung metastases
Hope is potentially on the horizon with a new treatment the thoracic surgery team at The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) has been trialling since October 2022. Known as robotic-assisted transbronchial microwave ablation of lung metastases, it is non-invasive and can treat these lung metastases without any surgical wounds, blood loss, pain or removal of healthy tissue. The new technology zeroes in on the cancer cells and destroys them, while minimising any procedural trauma to the patient.
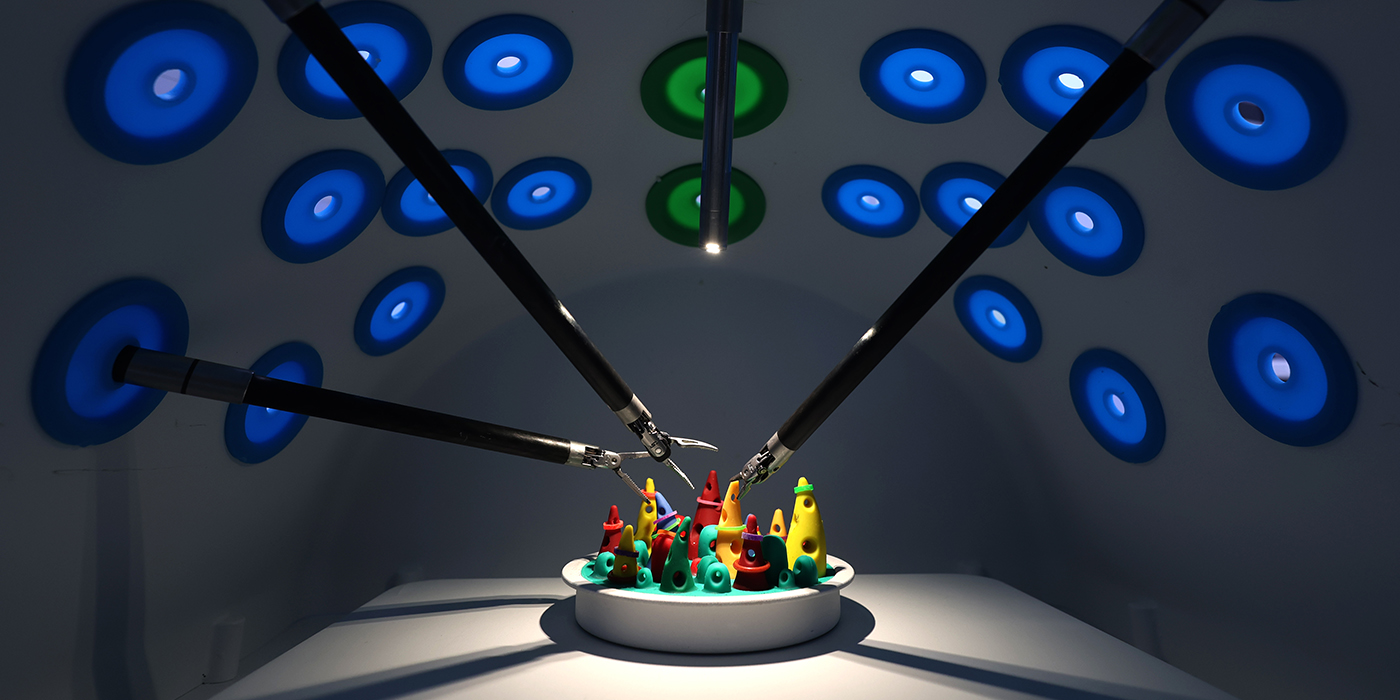
The procedure is driven by an advanced robotic navigation system, which is connected to a device known as a bronchoscope, delivering a 2mm wide catheter into the lung that can destroy the cancer cells using microwave energy. The design of the device was inspired by similar steerable catheters that are used for vascular procedures such as the insertion of stents. It’s operated remotely using a console linked to the bronchoscope; the operator can use real-time optical imaging and electromagnetic positioning to navigate their way through the airways within the lung.
The microwave energy is emitted by an antenna within the catheter. It’s delivered directly into the core of the cancer, minimising damage to peripheral lung tissue, with the amount of energy and duration of the treatment precisely tailored according to the needs of each patient and each individual metastasis. Compared to previous bronchoscopy systems, robotic-assisted procedure is more accurate in its navigation through the lungs and more stable when performing the procedure, increasing its effectiveness and decreasing the damage it causes.
“Operating the system involves placing a robotic-assisted bronchoscope onto the console’s two robotic arms,” says Dr Rainbow Lau Wing-hung, Clinical Assistant Professor (honorary) from the Division of Cardiothoracic Surgery, Department of Surgery at CU Medicine. “The operator is able to directly see a monitor displaying the view from the end of the bronchoscope as well as the generated navigation pathway and all the information necessary to guide them to the peripheral lung metastases. Using a small handheld controller, the operator can drive the bronchoscope robotically towards the targets.”
While the system currently requires human input, the team is looking into more automation in the navigation, potentially making it even more accurate.
Recovery from the procedure is straightforward: patients can resume normal diet few hours afterwards, they can generally resume normal activities as soon as they recover from the anaesthetic, and they only need to remain in hospital overnight for observation. About 80% experience no pain at all while the remaining can have mild pain that can easily be treated with painkillers.

Advantageous of navigation bronchoscopy
Navigation bronchoscopy is already used in a number of other procedures, says Professor Calvin Ng Sze-hang from the Division of Cardiothoracic Surgery, Department of Surgery at CU Medicine. “The main advantage of navigation bronchoscopy is the ability to accurately and quickly reach a lung lesion, usually in the more peripheral areas of the lung. Navigation bronchoscopy has been used in the past to obtain biopsy of a lung lesion for diagnosis; inject dye to mark a lesion and help surgeons identify it for resection during minimally invasive surgery; and place metal fiducial markers to guide precision radiotherapy.”
Three patients in Hong Kong have been treated with robotic-assisted transbronchial microwave ablation so far, all of them with stage 4 cancer, who had total of six metastases ablated. At over six months after the procedures were performed, the metastases show no sign of recurrence, and all three patients are doing well.
The procedure has since been successfully performed in Canada and the US. The team is currently involved in a multi-centre international trial using the system, which has already recruited more than 10 patients. Dr Lau says she expects to see more widespread clinical use of the system in around two years.
She adds the technology could also be adapted for use in diseases affecting other parts of the body. “The robotic-assisted navigation system is being investigated for its potential use in urology, given that a precision, robot-driven catheter can be beneficial in procedures such as kidney stone removal.”

The CU Medicine team’s work promises to make the treatment of some of the most painful and dangerous medical conditions simpler, less painful and more effective.